Continuing Medical Education Benefits
Obimages.net offers 18 Internet Based CME Courses. The total number of AMA PRA Category 1 Credit(s)™ is 26.95. All credits are accepted by the ARDMS. Quizzes and certificates are provided for each course.
$79 per year or $6.99 per month.
Continuing Medical Education jointly provided by the Minnesota Medical Association and Obimages.net


CME Statement
The Minnesota Medical Association designates these enduring materials for a maximum of 20 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Accreditation Statement:
This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of the Minnesota Medical Association and OBimages.net. The Minnesota Medical Association (MMA) is accredited by the ACCME to provide continuing medical education for physicians.
The total number of courses available is 15, which includes the following:
1.0 Credit: Twin Gestation: Overview
1.0 Credit: Twin Gestation: Complications
1.0 Credit: Fetal Doppler
1.25 Credits: Transvaginal Ultrasound of the Cervix
1.0 Credit: Introduction to Fetal Heart Scan
1.5 Credits: Ultrasound of Normal Fetal Heart Views
2.0 Credits: Diagnosis of Congenital Diaphragmatic Hernia
1.0 Credit: Fetal Chest: Pleural Effusion, Lymphangioma, Cystic Hygroma, and CHAOS
1.25 Credits: First Trimester: Normal and Abnormal
1.5 Credits: Placenta Accreta and Placenta Previa
1.5 Credits: Abruptio Placenta, Vasa Previa, and Chorioangioma
1.5 Credits: Umbilical Cord: Normal and Abnormal
1.5 Credits: Spina Bifida (Neural Tube Defects)
1.5 Credits: Gastroschisis and Omphalocele
1.5 Credits: Fetal Kidneys: Normal and Abnormal
Continuing Medical Education jointly provided by the Postgraduate Institute for Medicine (PMID) and Obimages.net


CME Statement
The Postgraduate Institute of Medicine designates these enduring materials for a maximum of 6.95 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
The total number of courses available is 3, which includes the following:
2,2 Credits: First Trimester Ultrasound including the Fetal Heart
3,0 Credits: Easy Diagnosis of Congenital Heart Defects
1.75 Credits: Stepwise Approach to the Complete Fetal Heart Exam
Literature Reviews
September 15, 2018
Comparison of diagnostic accuracy of early screening for pre-eclampsia by NICE guidelines and a method combining maternal factors and biomarkers: results of SPREE. Tan MY, Wright D, Syngelaki A, Akolekar R, Cicero S, JangaD, Singh M, Greco E, Wright A, Maclagan K, Poon LC, Nicolaides KH. Ultrasound Obstet Gynecol. 2018 Jun;51(6):743-750.
This study compared the performance of first-trimester screening for pre-eclampsia (PE) by a method that uses maternal factors with biomarkers to that of the current National Institute for Health and Care Excellence (NICE) guidelines. The performance of screening for pre-eclampsia as currently recommended by NICE guidelines is poor with low compliance compared to a method combining maternal factors with biomarkers.
August 25, 2018
Universal versus selective ultrasonography to screen for large-for-gestational-age infants and associated morbidity. Sovio U, Moraitis AA, Wong HS, Smith GCS. Ultrasound Obstet Gynecol. 2018 Jun;51(6):783-791.
This study sought to determine if ultrasound markers for large for gestational age (LGA) fetuses could identify at risk large for gestational age infants. Women underwent standard estimated fetal weight (EFW) assessment at around 36?weeks’ gestation (Universal sonography). This third trimester screening of nulliparous women increased the detection rate of LGA infants and, combined with ACGV (abdominal circumference growth velocity), identified those at risk for poor neonatal outcome. This is the first study to demonstrate the effectiveness of ultrasound estimated fetal weight combined with other ultrasound assessments in predicting adverse outcomes.
August 4, 2018
Preterm delivery after fetoscopic laser surgery for twin-twin transfusion syndrome: etiology and risk factors. Malshe A, Snowise S, Mann LK, Boring N, Johnson A, Bebbington MW, Moise KJ Jr, Papanna R. Ultrasound Obstet Gynecol. 2017 May;49(5):612-616.
This study sought to address the factors related to preterm delivery after fetoscopic laser surgery (FLS) for twin-twin-transfusion syndrome (TTTS). The results are from a single center reviewing 203 patients with TTTS who underwent FLS. The mean gestational age at FLS was 20.6 ±2.4 weeks with delivery occurring at 30.9?±?4.7?weeks. Preterm premature rupture of membranes (PROM) occurred in 39% of cases with spontaneous preterm delivery in 48%. Risk factors for spontaneous preterm delivery were iatrogenic preterm PROM, preoperative cervical length, and a number of anastomoses.
July 27, 2018
Increased nuchal translucency thickness and risk of neurodevelopmental disorders. Hellmuth SG, Pedersen LH, Miltoft CB, Petersen OB, Kjaergaard S, Ekelund C, Tabor A. Ultrasound Obstet Gynecol. 2017 May;49(5):592-598.
This study looked at the relationship between fetal nuchal translucency (NT) thickness and neurodevelopmental disorders in children with a normal chromosomal number. This study included 222,505 children who had undergone routine first trimester screening during fetal life. Children were divided according to prenatal NT and were followed-up to a mean age of 4.4?years. Follow-up information was obtained relative to intellectual disability, autism spectrum disorders (ASD), cerebral palsy, epilepsy, and febrile seizures. In summary, there was no increased risk of neurodevelopmental disorders among those with a first trimester NT 95(th)-99(th) percentile. Among children with a prenatal NT of >?99(th) percentile, the absolute risk of intellectual disability and ASD was reassuringly low (<?1%).
July 14, 2018
Early prediction of twin-to-twin transfusion syndrome: systematic review and meta-analysis. Stagnati, Zanardini, Fichera A, Pagani, Quintero RA, Bellocco, Prefumo F. Ultrasound Obstet Gynecol. 2017 May;49(5):573-582.
This study undertook an evaluation of the performance of certain first and second trimester markers to predict twin-to-twin transfusion syndrome (TTTS) in monochorionic twin gestations. Ultrasound parameters, measured before 16 weeks, were reviewed in 1991 such pregnancies. The following ultrasound parameters demonstrated an increased risk for the development of TTTS in monochorionic pregnancies: NT discrepancy, NT > 95th percentile; CRL (crown rump length) discrepancy >10%; abnormal ductus venosus flow on first trimester ultrasound.
June 25, 2018
Effect of maternal body mass index and amniotic fluid index on the accuracy of sonographic estimation of fetal weight in late gestation. Blitz MJ, Rochelson B, Stork LB, Augustine S, Greenberg M, Sison, CP, Vohra N. Am J Perinatol. 2018 Jan 10.
This study attempts to answer the effect of maternal weight (Maternal Body Mass Index, BMI) and Amniotic Fluid Index (AFI) on the accuracy of ultrasound Estimated Fetal Weight (EFW). In total, 1000 women were scanned between 40 to 42 weeks gestation over a three year period. In this retrospective analysis, the rate of error for EFW was increased in women with oligohydramnios, which was likely to overestimate fetal weight while polyhydramnios was likely to underestimate fetal weight. Maternal BMI did not affect fetal weight estimates during the gestational ages studied (40 to 41 weeks).
(Note: These studies seem to suggest the maternal weight does not correlate with the diagnosis of oligohydramnios but does correlate with higher rates of C-section. However, women with oligohydramnios are more likely to have errors in EFW, which contribute to over estimation of EFW while polyhydramnios seems to be associated with over estimates of EFW.)
April 24, 2018
Clinical experience with multigene carrier panels in the reproductive setting. Terhaar C, Teed N, Allen R, Dohany L, Settler C, Holland C, Longman. Prenat Diagn. 2018 Apr 23.
The American College of Obstetrics and Gynecology acknowledges that expanded carrier testing is an acceptable strategy to assess for genetic disorders. This study reported experience with three commercial laboratory panels with sizes varying from 3 to 218 disorders. The likelihood for identifying a carrier with a panel of 218 diseases was 36%. (Note: It is likely that prediction of genetic disorders will accelerate with the testing of potential carriers and expanding fetal testing.)
January 15, 2018
Outcome of monochorionic twin pregnancy with selective intrauterine growth restriction according to umbilical artery Doppler flow pattern of smaller twin: systematic review and meta-analysis. Buca D, Pagani G, Rizzo G, Familiari A, Flacco ME, Manzoli L, Liberati M, Fanfani F, Scambia G, D’Antonio F. Ultrasound Obstet Gynecol 2017;50:559-568.
This paper is a systematic review of monochorionic (MC) twin outcome among those with selective intrauterine growth restriction (sIUGR). Thirteen studies with 610 pregnancies were reviewed according to the umbilical artery Doppler waveform of the smaller twin. Classification is as follows: Type-1 sIUGR-fetuses with persistently positive Doppler flow, Type II-sIUGR with persistently absent/reversal flow, or Type III-sIUGR with intermittently absent/reversal flow. The authors found that Type I-sIUGR fetuses had more favorable outcomes compared to those with Type II and Type III. Lopriore’s editorial comment in the same issues points to unanswered questions related to management, type of sustained injury, and the need for prospective trials to study all aspects of MC fetuses with sIUGR.
December 13, 2017
Common findings in late-gestation fetal echocardiography. Tague L, Donofrio MT, Fulgium A, McCarter R, Limperopoulos C, Schidlow DN. J Ultrasound Med. 2017 Dec;36(12):2431-2437.
The purpose of the study was to identify and describe common cardiac findings in late gestation. Fetuses with hearts which were structurally normal were identified. Included were 40 fetuses between 24 and 38 weeks. The ratio of right sided measurements (tricuspid-to-mitral valve and right-to-left atrium ratios) were significantly increased in late gestation. Findings which generally increased after 34 weeks included: tapering of the ductus arteriosus, prominent aortic isthmus diastolic flow, prominent ductus arteriosus diastolic flow, trivial or mild tricuspid regurgitation, and aneurysms of the septum primum. These findings were deemed to be normal, following a physiologic trend manifest before birth.
October 29, 2017
Color and power Doppler combined with Fetal Intelligent Navigation Echocardiography (FINE) to evaluate the fetal heart. Yeo L, Romero R. Ultrasound Obstet Gynecol. 2017 Oct;50(4):476-491.
The authors evaluated the use of color bidirectional power Doppler ultrasound combined with Fetal Intelligent Navigation Echocardiography (FINE) to examine the fetal heart. One or more spatiotemporal image correlation (STIC) volume datasets were obtained in 169 normal fetal hearts in 37 patients. In addition, data sets were obtained in four cases of congenital heart defects. The FINE method or technology (Samsung Healthcare, ultrasound platform UGEO WS80A) was applied to the STIC volume data sets using only 1 standard plane, which generates eight to nine standard fetal echocardiography views (via grayscale, color Doppler, or power Doppler) in the second and third trimesters. Using 1 diagnostic plane, color Doppler FINE generated 9 fetal echocardiography views (grayscale) in 73% to 100% of cases. The rate of generating 8 successful views with appropriate color was 89% to 99% and was 91% to 100% with S-flow Doppler information. The success rate for the ninth view (venae cavae) was less, 30% to 33%. In summary, the FINE method successfully generated 8 to 9 echo fetal cardiac views using 1 diagnostic plane and was successful in identifying abnormal cardiac anatomy in all malformations studied. Below: Example of Tetralogy of Fallot obtained with FINE technology with 1 standard plane generating 9 fetal echo views.
October 17, 2017
Association of chronic hypertension with birth of small-for-gestational-age neonate. Panaitescu AM, Baschat AA, Akolekar R, Syngelaki A, Nicolaides KH. Ultrasound Obstet Gynecol. 2017 Sep;50(3):361-366.
The purpose of the study was to determine the effect of chronic hypertension on the incidence of small-for-gestational-age (SGA) infant in the absence of superimposed pre-eclampsia. The study population included 1052 women with chronic hypertension and 73,174 without chronic hypertension. In addition to medical characteristics and medical history, mean arterial pressure was measured at 11-13 weeks.
Preeclampsia developed in 22.1% of those with chronic hypertension and pre-eclampsia developed in 2.3% of those without chronic hypertension. In the group with chronic hypertension, the incidence of SGA in the pregnancies that developed preeclampsia was 10.3% and the incidence of SGA in the pregnancies that did not develop preeclampsia was 5.7%. The association of chronic hypertension with the subsequent development of preeclampsia contributes to the increased risk of SGA in pregnancies with chronic hypertension.
August 31, 2017
Early diagnosis of bladder exstrophy: quantitative assessment of a low-inserted umbilical cord. Fishel-Bartal M, Perlman S, Messing B, Bardin R, Kivilevitch Z, Achiron R, Gilboa Y. J Ultrasound Med. 2017 Sep:1801-1805.
The diagnosis of bladder exstrophy, a rare congenital anomaly, is difficult. These authors describe a technique to assess for this condition at less than 18 weeks’ gestation. If the urinary bladder was not visualized, the authors measured the length between the umbilical cord insertion and the genital tubercle. The measurement was taken in the midsagittal plane, similar to a nuchal translucency assessment, and the fetus was kept in a neutral position. Using this technique, all 6 cases of bladder exstrophy were diagnosed. The criteria for diagnosis is the umbilical cord insertion to the genital tubercle length of below the fifth percentile for gestational age. A normative chart for these measurements is provided in the published report.
August 14, 2017
Increased nuchal translucency thickness and risk of neurodevelopmental disorders. Hellmuth SG, Pedersen LH, Miltoft CB, Petersen OB,Kjaergaard S, Ekelund C, Tabor A. Ultrasound Obstet Gynecol. 2017 May;49(5):592-598.
This study looked at the relationship between fetal nuchal translucency (NT) thickness and neurodevelopmental disorders in children with normal chromosomal number. The data included 222,505 children who had undergone routine first trimester screening during fetal life. Children were divided according to prenatal NT and were followed-up to a mean age of 4.4?years. Follow-up information was obtained relative to intellectual disability, autism spectrum disorders (ASD), cerebral palsy, epilepsy, and febrile seizures. In summary, there was no increased risk of neurodevelopmental disorders among those with a first trimester NT 95(th)-99(th) percentile. Among children with a prenatal NT of >?99(th) percentile, the absolute risk of intellectual disability and ASD was reassuringly low (<?1%).
July 19, 2017
Preterm delivery after fetoscopic laser surgery for twin-twin transfusion syndrome: etiology and risk factors. Malshe A, Snowise S, Mann LK, Boring N, Johnson A, Bebbington MW, Moise KJ Jr, Papanna R. Ultrasound Obstet Gynecol. 2017 May;49(5):612-616.
This study sought to address the factors related to preterm delivery after fetoscopic laser surgery (FLS) for twin-twin-transfusion syndrome (TTTS). The results are from a single center reviewing 203 patients with TTTS who underwent FLS. The mean gestational age at FLS was 20.6 ±2.4 weeks with delivery occurring at 30.9?±?4.7?weeks. Preterm premature rupture of membranes (PROM) occurred in 39% of cases with spontaneous preterm delivery in 48%. Risk factors for spontaneous preterm delivery were iatrogenic preterm PROM, preoperative cervical length, and number of anastomoses.
July 10, 2017
Early prediction of twin-to-twin transfusion syndrome: systematic review and meta-analysis. Stagnati, Zanardini, Fichera A, Pagani, Quintero RA, Bellocco, Prefumo F. Ultrasound Obstet Gynecol. 2017 May;49(5):573-582.
This study undertook an evaluation of the performance of certain first and second trimester markers to predict twin-to-twin transfusion syndrome (TTTS) in monochorionic twin gestations. Ultrasound parameters, measured before 16 weeks, were reviewed in 1991 such pregnancies. The following ultrasound parameters demonstrated an increased risk for the development of TTTS in monochorionic pregnancies: NT discrepancy, NT > 95th percentile, CRL (crown rump length) discrepancy > 10%, and abnormal ductus venosus flow on first trimester ultrasound.
June 17, 2017
The role of early gestation ultrasound in the assessment of fetal anatomy in maternal obesity. Romary L, Sinkovskaya E, Ali S, Cunningham TD, Marwitz S, Heeze A, Herlands L, Porche L, Philips J, Abuhamad A. J Ultrasound Med. 2017 Jun;36(6):1161-1168.
A 2012 consensus suggested that ultrasound examinations in obese patients should be performed at 20 to 22 weeks and when anatomy is incomplete, a follow-up scan should be performed in 2 to 4 weeks. The question posed by this study was: Could imaging performed earlier in the pregnancy improve visualization of fetal structures? In obese patients with a BMI of > 30, with a singleton gestation, and no karyotype abnormality, an ultrasound performed at (13?+?0 to 15?+?6 weeks) and was compared with the traditional second trimester ultrasound. This obese group was compared to women with a singleton gestation, no karyotype abnormality, age > than 18 years, at < 16 weeks’ gestation, and with a BMI of less than 30. Both groups underwent a transvaginal and/or transabdominal sonogram for fetal anatomic survey at 13?+?0 to 15?+?6 weeks’ gestation (US1). Those in the study also underwent a transabdominal sonogram at 18 to 24 weeks (US2). A repeat transabdominal sonogram (2-US2) was performed 2 to 4 weeks later if US1 failed to detail anatomy. In summary, the authors found that the highest benefit for the addition of an early ultrasound was for women with Class III obesity (BMI?>?40?kg/m(2).
June 5, 2017
Zika virus vaccines: a full field and looking for the closers. Thomas SJ. N Engl J Med 2017; 376:1883-1886.
This article discusses testing Zika virus vaccines. The article cites two studies of messenger RNA Zika virus vaccines, which show protection against infection in animal models. While research and development to date has been impressive, it is not clear whether the Zika virus acts like a flavivirus or dengue virus. If it acts like a flavivirus, chances for successful vaccine development may be greater. The goal is to protect women from the Zika virus through active immunization. However, at this time, active research continues towards developing an effective vaccine.
June 5, 2017
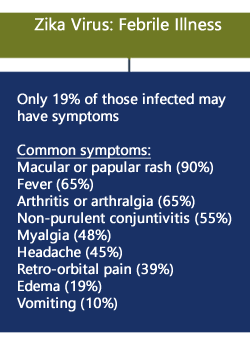
Cutaneous eruption in a U.S. woman with locally acquired Zika virus infection. Chen L, et. al. N Engl J Med 2017; 376:400-401.
In summary, this is a case report of acquired Zika virus in a pregnant woman who had not traveled outside of the United States. Positive findings at 23 weeks gestation were: erythematous follicular macules and papules on the trunk and arms, scattered tender pink papules on the palms, and a few petechial lesions on the hard palate. Histology of the skin lesion showed: a mild perivascular lymphocytic infiltration in the upper dermis, admixed with some neutrophils. ZIKV RNA was detected in both urine and serum specimens, using a reverse-transcriptase polymerase chain reaction (RT-PCR). Occurring in Florida, this is the first non-travel-associated case of ZIKV infection in the United States.
May 4, 2017
Utility of ultrasound examination at 10-14 weeks prior to cell-free DNA screening for fetal aneuploidy. Vora KL, Robinson S, Hardisty EE, Stami DM. Ultrasound Obstet Gynecol. 2017;49(4):465-469.
In this study, 1806 women with advanced maternal age (AMA) underwent a 10-14 week ultrasound study and aneuploidy screening, 68.5% of whom selected cell-free DNA screening. Among these women, 16.1% had an ultrasound finding such as anomaly, incorrect dating, multiple gestation, and non-viable pregnancy which may have altered recommendations as to the screening or testing decisions. The authors recommend a 10 to 14 week ultrasound study prior to cell-free DNA testing in AMA women.
May 5, 2017
Diagnostic accuracy of individual antenatal tools for prediction of small-for-gestational age at birth. Poljak B, Agarwal U, Jackson R, Alfirevic Z, Sharp A. Ultrasound Obstet Gynecol. 2017 Apr;49(4):493-499.
A number of fetal and newborn growth charts for estimated fetal weight (EFW) were compared to assess the accuracy of these charts at < 10th percentile to predict small-for-gestational age (SGA) at birth. The various ultrasound charts assessed were among those pregnancies excluded on the basis of abnormal Doppler. The authors cite wide variation in the accuracy to predict the SGA fetus and to predict adverse perinatal outcome. All of the present EFW charts have low rates of detection for SGA. The authors suggest using a combination of fetal biometry and EFW with placental biomarkers to detect SGA and adverse perinatal outcome.
March 7, 2017
Accuracy of sonographically estimated fetal weight near delivery in pregnancies complicated with diabetes mellitus. Valent AM, Newman T, Kritzer S, Magner K, Warshak CR. J Ultrasound Med. 2017 Mar;36(3):593-599.
The study’s purpose was to evaluate the accuracy of ultrasound estimated fetal weight (FW) within 2 weeks of delivery and the signed percent error (the mean ± standard deviation) between patients with and without Diabetes. The study population was composed of 6843 births. The authors found no significant difference between the two groups for the accuracy of estimated FW near delivery or of signed percent error. Sonography had a high specificity (the extent to which estimated FW really represents birth weights of greater than 4000 grams)
January, 2017
Longitudinal assessment of examiner experience and the accuracy of sonographic fetal weight estimation at term. Faschingbauer F, Heimrich J, Raabe E, Kehl S, Schneider M, Schmid M, Beckmann MW, Hepp T, Lübke A, Mayr A, Schild RL. J Ultrasound Med. 2017;36(1):163-174.
This study seeks to assess the influence of the ultrasound scanner’s experience on the accuracy of ultrasound estimation of weight and to analyze the scanner’s individual learning curves. This was a multi-center study in which 4613 ultrasound weight estimations were performed by 18 examiners at the beginning of their ultrasound training. Variables to determine ultrasound errors were applied, and the examiner’s experience was evaluated including the number of examinations. In addition, the individual learning curves of the examiners was determined. After adjustments, there was a significant influence related to the number of examinations on the accuracy of sonographic weight estimation (P?<?.001). A typical learning curve with improving accuracy was found at approximately 200 examinations. The diagnostic performance started to deteriorate again between 200 and 300 examinations. The authors stress the importance of continuous quality control for ultrasound weight estimation.
December, 2016
Cervical cerclage for preterm birth prevention in twin gestation with short cervix: a retrospective cohort study. Houlihan C, Poon LC, Ciarlo M, Kim E, Guzman ER, Nicolaides KH. Ultrasound Obstet Gynecol. 2016;48(6):752-756.
The purpose of the study was to determine whether the application of cervical cerclage reduces the rate of premature birth in dichorionic diamniotic (DCDA) twins who have a short cervix detected by ultrasound. In 40 consecutive DCDA twin gestations, cervical cerclage was performed for an ultrasound derived cervical length of 1-24 mm at 16-24 weeks’ gestation. There were 40 control patients who did not undergo cerclage and who were matched for gestational age and cervical length with the cerclage group. In the cases with cerclage application compared with controls, spontaneous delivery < 32 weeks was significantly less frequent (20.0% vs 50.0%; relative risk, 0.40 (95% CI, 0.20-0.80)). Women who underwent cerclage were less likely to spontaneously deliver at < 32 weeks. In summary, in DCDA twin gestation with a short cervix, treatment with cervical cerclage may reduce the rate of early preterm birth. The authors suggest the need for further adequate randomized controlled trials on cerclage in twin gestations with a short cervix.
November, 2016
Prediction of stillbirth from biochemical and biophysical markers at 11-13 weeks. Mastrodima S, Akolekar R, Yerlikaya , Tzelepis T, Nicolaides KH. Ultrasound Obstet Gynecol. 2016;48(5):613-617.
Prediction of stillbirth at 11 to 13 weeks was based upon a model which combined maternal characteristics and maternal medical history with first trimester biochemical and biophysical markers. The study’s objectives were to evaluate how the screening by this model was predictive for all stillbirths and those due to impaired placentation and to unexplained causes. In this study 76,897 singleton pregnancies were screened. Among these, there were 268 (0.35%) antepartum stillbirths. Among the stillbirths, 59% were due to impaired placentation and 41% were due to other or unexplained causes. Multivariable logistic regression analysis considered the following factors: maternal factor-derived a-priori risk, fetal nuchal translucency thickness, ductus venosus pulsatility index for veins (DV-PIV), uterine artery pulsatility index (UtA-PI), and maternal serum free ?-human chorionic gonadotropin and pregnancy-associated plasma protein-A (PAPP-A). A model combining these variables predicted 40% of all stillbirths and 55% of those due to impaired placentation, with a false-positive rate of 10%. The authors stress that prevention of stillbirths remains to be determined.
October, 2016
Neonatal outcomes in fetuses with a persistent intrahepatic right umbilical vein. Canavan TP, Hill LM. J Ultrasound Med. 2016;35(10):2237-2241.
Persistent right umbilical vein may be associated with abnormal findings in the fetus or may be a normal finding. In this study, 313 fetuses were noted on the 17 to 24 week ultrasound to have a persistent right umbilical vein identified, which was defined as a left curving umbilical vein passing to the right of a medially displaced gall bladder. An adverse event was defined as aneuploidy, fetal demise, or neonatal death. A normal neonatal outcome was reported in 69.3% (217 patients). Adverse outcomes included 5 fetuses with aneuploidy, and 24 fetuses with major anomalies. There were 2 neonatal deaths and 1 fetal demise. In the presence of a persistent intrahepatic right umbilical vein, the authors stress the importance of a complete anatomic and cardiac evaluation with further appropriate referral as needed.
August 10, 2016
Role of 3-vessel and trachea view in the diagnosis of tetralogy of fallot. Palatnik A, Grobman WA, Cohen LS, Dungan JS, Gotteiner NL. J Ultrasound Med. 2016 Aug;35(8):1799-809.
The role of the 3 vessel and trachea view in the prenatal diagnosis of Tetralogy of Fallot (TOF) is addressed in a recent article. The diagnostic frequency of TOF is low (32% to 47%) and methods to improve accuracy are pursued. Despite the classic anatomic defects of override of the aortic root over a ventricular septal defect (VSD) and infundibular pulmonary stenosis, the diagnosis is often missed. In this study, the 3 vessel and trachea view was abnormal in TOF and on that view, the single most important marker is an enlarged aortic arch isthmus compared to the pulmonary artery. Normally the pulmonary artery is larger than the aorta and the pulmonary valve is larger than the aortic valve, but in TOF, the aortic valve is larger than the pulmonary valve. These findings were present in all fetuses with TOF on the 3-vessel trachea view.

June 20, 2016
Prediction of spontaneous preterm birth among nulliparous women with a short cervix. Grobman WA, et. al. J Ultrasound Med. 2016 Jun;35(6):1293-7
The object of the study was to determine whether women with a short cervix (cervical length of < 30 mm) could be included in an accurate prediction model for preterm birth if additional demographic and sonographic factors were included in the model. A secondary analysis was performed of trials among women with a cervical length of < 30 mm obtained at 16 to 22 weeks who did not have other risk factors for spontaneous or medically indicated preterm birth. Risk factors known to be associated with spontaneous preterm birth were included in a regression analysis to determine if these factors could improve prediction in women with a cervical length of < 30 mm. Despite inclusion of these risk factors in those women with a short cervix, an accurate prediction model could not be developed. Furthermore, according to the authors, at 16 to 22 weeks gestation, the 10th percentile for cervical length is 30 mm. Among women in the United States, the risk for preterm birth in this group is 25%.
April 23, 2016
Accuracy of ultrasound in the antenatal detection of placental disorders. Pilloni E, et. al. Ultrasound Obstet Gynecol. 2016 Mar;47(3):302-7.
The purpose of the study was to determine the accuracy of ultrasound in the detection of placenta accreta and the effect on outcome as it relates to prenatal diagnosis. Among 314 patients prospectively studied with suspected placenta previa, 37 met ultrasound criteria for placenta accreta. Detection rates for placenta accreta were better in the presence of an anterior placenta (89.7%) compared to women with a posterior placenta (50%). Women who had a placental attachment disorder diagnosed prenatally had less blood loss and shorter hospitalization. Gray scale and color had good overall performance for the diagnosis of placenta accreta.
April, 2016
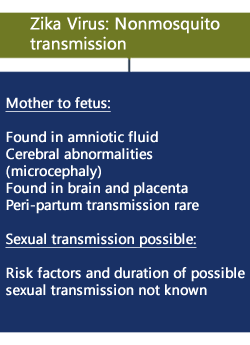
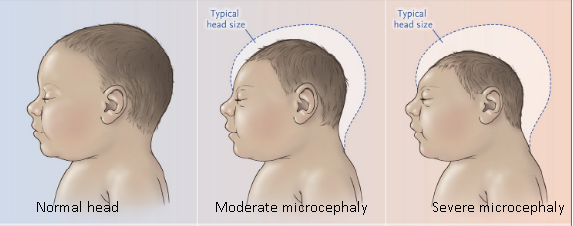
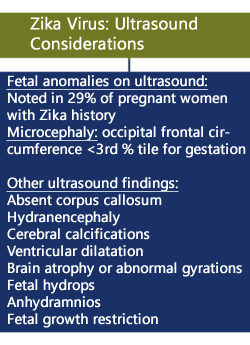
Zika Virus. Petersen LR, Jamieson DJ, Powers AM, Honein MA. N Engl J Med. 2016 Apr 21;374(16):1552-63.
A summary of key findings in a review of the Zika Virus is provided below.
April, 2016
Prospective evaluation of the fetal heart using Fetal Intelligent Navigation Echocardiography (FINE). Garcia M, et. al. Ultrasound Obstet Gynecol. 2016 Apr;47(4):450-9.
The following is a brief review of a new diagnostic method in fetal heart ultrasound called “Fetal Intelligent Navigation Echocardiography” (FINE). The study presents the results of acquired heart volumes from a single orientation of the fetal heart. “The FINE method can be applied to generate nine standard fetal echocardiography views.” The study shows successful acquisitions of the 9 fetal heart views in 72.5% of the normal heart cases. The use of FINE is already commercially available.
April, 2016
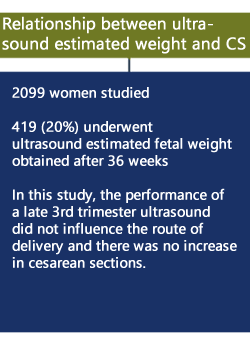
Relationship between third-trimester sonographic estimate of fetal weight and mode of delivery. Yee LM, Grobman WA. J Ultrasound Med. 2016 Apr;35(4):701-6
The following is a brief review of a clinical study on estimated fetal weight and Cesarean delivery. The study indicates that ultrasound estimated fetal weight performed after 36 weeks gestation does not appear to influence the decision to perform Cesarean section.
March 26, 2016
Correlation between cervical lengths measured by transabdominal ultrasound and transvaginal ultrasound for the prediction of preterm birth. Cho HJ, Roh HJ. J Ultrasound Med. 2016 Mar;35(3):537-44.
Due to the potential discomfort of transvaginal ultrasound, this study sought to determine whether the result of a transabdominal ultrasound measurement of cervical length could determine which women should undergo transvaginal ultrasound in order to predict preterm birth. In this prospective study, measurements of cervical length were taken between 20 and 29 weeks gestation. Transabdominal ultrasound cervical lengths which are not measureable or < 2.0 cm or < 2.5 cm indicate the need for transvaginal ultrasound for the prediction of premature birth, while women whose cervix is measurable and long on transabdominal ultrasound may not require transvaginal ultrasound for prediction purposes.
March 15, 2016
Interim Guidance on ultrasound for Zika virus infection in pregnancy: information for healthcare professionals. Papageorghiou AT, et. al. Ultrasound Obstet Gynecol 2016;47:530-532.
The International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) has published an article about interim guidance on ultrasound for Zika virus infection during pregnancy. This guidance report acknowledges the potentially valuable information which may be obtained by ultrasound practitioners.
March 2, 2016
Trying to conceive after an early pregnancy loss: an assessment on how long couples should wait. Schliep KC, et. al. Obstet Gynecol. 2016 Feb;127(2):204-12.
Among couples trying to conceive after different intervals of pregnancy loss, the study assessed the time to pregnancy and live birth. The population consisted of 1083 women, aged 18 to 40 years with one or two early pregnancy losses. Couples with a 0 to 3 month interval (76.7%) compared to a greater than 3 month interval (23.4%) were more likely to achieve live birth with a significantly shorter time to pregnancy. The authors conclude “there is no physiologic evidence for delaying pregnancy attempt after an early loss.”
February 17, 2016
Cervical length and quantitative fetal fibronectin to predict spontaneous preterm labor (sPTL) in asymptomatic high-risk women. Kuhrt K, Smout E, Hezelgrave N, Seed PT, Carter J, Shennan AH. Ultrasound Obstet Gynecol. 2016 Jan;47(1):104-9.
Quantification of fetal fibronectin, cervical length measurements, and one or more high-risk clinical historical factors were used to construct a predictive tool for spontaneous preterm labor (sPTL) in high-risk women. The final model was predictive of sPTL and the areas under the receiver-operating curves ranged from 0.77 to 0.99 suggesting accurate predictions across five delivery outcomes.
February 8, 2016
Comparison of Solomon technique with selective laser ablation for twin-twin transfusion syndrome: a systematic review. Dhillon RK, Hillman SC, Pounds R, Morris RK, Kilby MD. Ultrasound Obstet Gynecol. 2015 Nov;46(5):526-33.
This study is a systematic review of 2 cohort studies and 1 randomized controlled trial (RCT) comparing these two techniques for the treatment of twin-twin transfusion syndrome (TTTS) in diamniotic monochorionic twins. The findings suggest that the Solomon technique is associated with a trend towards reduction in TAPS (Twin Anemia-Polycythemia Sequence) and recurrent TTTS, while survival is increased without adverse effects or events. The authors suggest the need for further RCTs with long-term neurological follow-up.
January 29, 2016
Interim guidelines for pregnant women during a Zika virus outbreak – United States, 2016. Petersen EE, Staples JE, Meaney-Delman D, Fischer M, Ellington SR, Callaghan WM, Jamieson DJ. MMWR Morb Mortal Wkly Rep. 2016 Jan 22;65(2):30-3.
Pregnant women with a history of travel to an area with Zika virus transmission and who report two or more symptoms consistent with Zika virus disease (acute onset of fever, maculopapular rash, arthralgia, or conjunctivitis) during or within 2 weeks of travel, or who have ultrasound findings of fetal microcephaly or intracranial calcifications, should be tested for Zika virus infection in consultation with their state or local health department.
Maternal-fetal transmission of Zika virus has been documented throughout pregnancy. Zika virus RNA has been detected in the pathologic specimens of fetal losses. In the current outbreak in Brazil, a marked increase in the number of infants born with microcephaly has been reported. However, it is not known how many of the microcephaly cases are associated with Zika virus infection.
There is neither a vaccine nor prophylactic medications available to prevent Zika virus infection. The CDC recommends that all pregnant women consider postponing travel to areas where Zika virus transmission is ongoing. If a pregnant woman travels to an area with Zika virus transmission, she should be advised to strictly follow steps to avoid mosquito bites.
January 27, 2016
What is the rate of incomplete fetal anatomic surveys during a second-trimester scan? Retrospective observational study of 4000 nonobese pregnant women. Padula F, et. al. J Ultrasound Med. 2015 Dec;34(12):2187-91.
Among 4000 women who underwent a second trimester scan, a small percentage were incomplete due to unfavorable fetal position. Among the study population, 4.2% returned for a follow-up scan within 2 weeks. Only 1 view was need in a subsequent scan in 2.6%, while 1.6% required more than 1 view. The most difficult organs to visualize during the initial scan were: corpus callosum (1.8%), fetal face (1.7%), cerebellar vermis (1.1%), and fetal heart (1.0%).
January 1, 2016
Sonographic detection of growth restriction in pregnancies with gastroschisis. Nelson DB, Martin R, Twickler DM, Santiago-Munoz PC, McIntire DD, Dashe JS. J Ultrasound Med. 2015 Dec;34(12):2217-23.
A retrospective cohort study was performed, assessing 111 births with gastroschisis. Growth restriction was diagnosed using Hadlock’s nomogram and was defined as an estimated fetal weight of less than the 10th percentile for gestational age. The sensitivity and negative predictive value for the sonographic prediction of the small for gestational age neonate was 90% by 32 weeks and approximately 95% after 32 weeks. A low birth weight percentile on the antenatal scan was not associated with an immediate increase in neonatal morbidity or mortality.
December 22, 2015
Second-trimester cervical length as risk indicator for Cesarean delivery in women with twin pregnancy. van de Mheen L, et. al. Ultrasound Obstet Gynecol. 2015 Nov;46(5):579-84.
In this study, 311 women with a twin gestation attempted vaginal delivery after 34 weeks. Second trimester cervical length was measured in these women to determine if there were an association with the risk of emergency Cesarean section. In nulliparous women, there was no relationship between second-trimester CL and Cesarean delivery.
December 8, 2015
Accuracy of three-dimensional ultrasound compared with magnetic resonance imaging in diagnosis of Müllerian duct anomalies using ESHRE-ESGE consensus on the classification of congenital anomalies of the female genital tract. Graupera B, Pascual MA, Hereter L, Browne JL, Úbeda B, Rodríguez I, Pedrero C. Ultrasound Obstet Gynecol. 2015 Nov;46(5):616-22.
Three-dimensional (3-D) ultrasound compared with magnetic resonance imaging (MRI) in the diagnosis of Müllerian duct anomalies is highly accurate. [1] After being suspected of a uterine anomaly on two-dimensional scanning, 60 women were evaluated with 3-D ultrasound and with MRI. Compared with MRI, 3-D ultrasound had a sensitivity of 100% for dysmorphic uteri, and the kappa was 1.00. For hemi-uteri, the sensitivity was 100%, and the kappa was 1.00. For septate uteri, the sensitivity was 100%, and the kappa was 0.918. For bicorporeal uteri, the sensitivity was 83.3%, and the kappa was 0.900. Therefore, 3-D ultrasound is highly accurate for diagnosing uterine malformations, and it also has a good level of agreement with MRI in the classification of different anomalies.
November 28, 2015
A randomized trial of progesterone in women with recurrent miscarriages. Coomarasamy A, et. al. N Engl J Med. 2015 Nov 26;373(22):2141-8.
A multicenter, double-blind, placebo-controlled, randomized trial was undertaken in 836 women. The aim was to determine whether supplementation with progesterone in the first trimester of pregnancy would increase the rate of live births among women with a history of unexplained recurrent miscarriages. Women were randomly assigned to receive either twice-daily vaginal suppositories containing either 400 mg of micronized progesterone or matched placebo. In women with a history of unexplained recurrent miscarriages, progesterone therapy did not result in higher rates of live births.
November 25, 2015
Analysis of cell-free DNA in maternal blood in screening for fetal aneuploidies: updated meta-analysis. Gil MM, Quezada MS, Revello R, Akolekar R, Nicolaides KH. Ultrasound Obstet Gynecol. 2015 Mar;45(3):249-66.
A total of 37 studies were used for the meta-analysis. Trisomy 21 screening by cell-free DNA is superior to all methods of screening with a higher detection rate (DR) and a lower false positive rate (FPR), which leads to fewer unnecessary invasive procedures.c The detection rate of screening by cell-free DNA for trisomies 18, 13, and sex chromosome aneuploidies is lower than that for Trisomy 21. The authors do not suggest screening for fetal trisomies 18 and 13 independently from Trisomy 21 screening. While universal screening is associated with high costs, cell-free DNA testing contingent upon the results from first trimester ultrasound and biochemical testing is a strategy suggested by the authors.
November 9, 2015
Precesarean prophylactic balloon catheters for suspected placenta accreta: a randomized controlled trial. Salim R, Chulski A, Romano S, Garmi G, Rudin M, Shalev E. Obstet Gynecol. 2015 Nov;126(5):1022-8.
Twenty seven women were randomized to an intervention groups (13) who underwent prophylactic balloon catheter placement for suspected placenta accreta and 14 control patients who did not undergo placement. The outcome measure was the number of packed red blood cell units transfused, which did not differ between the two groups. Two of 13 women (15.4%) in the treatment group had reversible adverse effects. This is one of the few studies to address this issue and the authors acknowledge the small sample size and emphasize the difference between prophylaxis and treatment of postpartum hemorrhage by arterial embolization, which has been shown to be effective.
October 30, 2015
Middle cerebral artery peak systolic velocity predicts fetal hemoglobin levels in twin anemia-polycythemia sequence. Slaghekke F, et. al. Ultrasound Obstet Gynecol. 2015 Oct;46(4):432-6.
TAPS is a syndrome in monochorionic twin pregnancies resulting in the inter-twin transfusion of blood via small anastomosis. Occurring in approximately 13% of post laser treatment of twin to twin transfusion syndrome, TAPs results in significant hemoglobin differences between twins in the absence of evidence for oligohydramnios or polyhydramnios. A recent paper records 116 MCA-PSV measurements in 74 donors and 42 recipients with TAPS. In fetuses with TAPS, MCA-PSV is diagnostic for predicting abnormal hemoglobin levels.
October 16, 2015
Prenatal detection of congenital heart defects at the 11- to 13-week scan using a simple color Doppler protocol including the 4-chamber and 3-vessel and trachea views. Wiechec M, Knafel A, Nocun A. J Ultrasound Med. 2015 Apr;34(4):585-94.
In this prospective observational study performed at 11 to 13 weeks among 1084 patients, 35 cases were confirmed to have a congenital heart defect. The most effective approach was color mapping of the 4-chamber and 3-vessel and trachea views. The ideal insonation beam was 45 degrees with the fetal spine at 6 o’clock. The transducer assessed ventricular inflows in color at the level of the 4-chamber view, the 3-vessel view, and finally demonstrating the V sign at the level of the 3-vessel trachea view. Using this approach, a sensitivity of 88.5% and a specificity of 100% for the detection of CHD at 11 to 13 weeks was achieved. In addition, the vascular patterns for many of the defects are presented.
October 16, 2015
Prevention of postpartum hemorrhage and hysterectomy in patients with morbidly adherent placenta: a cohort study comparing outcomes before and after introduction of the Triple-P procedure. Teixidor Viñas M, Belli AM, Arulkumaran S, Chandraharan E. Ultrasound Obstet Gynecol. 2015 Sep;46(3):350-5.
The Triple-P procedure is a surgical method intended to reduce postpartum hemorrhage and hysterectomy in cases of placenta accreta, including placenta increta and percreta. Step 1 involves placental localization and delivery of the fetus via a transverse uterine incision above the upper margin of the placenta. Step 2 involves the inflation of pre-operatively placed occlusion balloons into both internal iliac arteries. In Step 3, the placenta is not separated and myometrial excision and reconstruction of the uterine wall is performed. If the bladder is invaded (percreta), the placenta is left in situ and hemorrhagic areas are treated with hemostatic powder. The Triple-P procedure resulted in reduced hysterectomy, post partum hemorrhage, and hospital stay among a small cohort of patients. The authors acknowledge the need for further multicenter studies to confirm improved outcomes. Further, this procedure should be attempted only in centers with high levels of expertise among multiple disciplines.
July, 2015
Prediction of small-for-gestational-age neonates: screening by uterine artery Doppler and mean arterial pressure at 30-34 weeks. Bakalis S, Stoilov B, Akolekar R, Poon LC, Nicolaides KH. Ultrasound Obstet Gynecol. 2015 Jun;45(6):707-14.
Prediction of small-for-gestational-age neonates: screening by fetal biometry at 35-37 weeks. Fadigas C, Saiid Y, Gonzalez R, Poon LC, Nicolaides KH. Ultrasound Obstet Gynecol. 2015 May;45(5):559-65.
Combined maternal characteristics and fetal biometry were used to predict SGA at 30-34 weeks. In the absence of preeclampsia (PE), maternal characteristics associated with SGA included increased inter-pregnancy interval, decreased height and weight, certain racial origins, cigarette smokers, prior history of SGA, and chronic hypertension. In the absence of PE, the Z-scores* of head circumference (HC), abdominal circumference (AC), femur length (FL), or estimated fetal weight (EFW) were reduced at 30 to 34 weeks gestation. Using these criteria, 80% of SGA neonates at < 10th percentile delivering at preterm with SGA were identified with a false positive rate of 10%.
*z Score: A z-score (aka, a standard score) indicates how many standard deviations an element is from the mean. A z-score can be calculated from the following formula. z = (X – ?) / ? where z is the z-score, X is the value of the element, ? is the population mean, and ? is the standard deviation.
The same methodology is used in the study to predict SGA neonates at 35-37 weeks. Similar maternal characteristics were noted at 35-37 weeks and combined with fetal biometry (EFW Z-scores), 90% of pregnancies were identified that delivered a SGA neonate within 2 weeks of assessment with a false positive rate of 10%. In addition, 70% of SGA neonates were predicted that delivered at ? 37 weeks.
June, 2015
Systematic review of accuracy of ultrasound in the diagnosis of vasa previa. Ruiter L, et. al. Ultrasound Obstet Gynecol. 2015 May;45(5):516-22.
A recent systematic review of the accuracy of ultrasound in the diagnosis of vasa previa included 583 articles of which two were prospective and six were retrospective cohort studies. Whether transvaginal ultrasound (TVS) is used for primary evaluation or for evaluation after vasa previa is suspected on transabdominal scan, TVS with color Doppler is the superior method for evaluation. Transvaginal color Doppler in the second trimester resulted in 100% sensitivity and 99.0 to 99.8% sensitivity.
June, 2015
Prediction of early- and late-onset pregnancy-induced hypertension using placental volume on three-dimensional ultrasound and uterine artery Doppler. Arakaki T, et. al. Ultrasound Obstet Gynecol. 2015 May;45(5):539-43.
Increased uterine artery resistance and small placental volume as measured by 3-D ultrasound placental volume at 11 to 13 weeks is associated with the development of early PIH, but is not associated with the development of late onset PIH. In early onset PIH, both neonatal weight and placental weight were lower, while there was no difference in the late onset PIH group and unaffected pregnancies, suggesting that early and late PIH may be different entities.
June, 2015
Longitudinal assessment of lung area measurements by two-dimensional ultrasound in fetuses with isolated left-sided congenital diaphragmatic hernia. Ruano R, et. al. Ultrasound Obstet Gynecol. 2015 May;45(5):566-71.
Two-dimensional (2D) ultrasound was used for fetal right lung measurements between 19 and 37 weeks in healthy fetuses and those with isolated left-sided CDH. Right lung areas were measured by tracing and longest diameter methods and thereafter a lung area-to-head circumference ratio (LHR) was calculated. Compared to healthy fetuses, those with CDH demonstrated a significantly slower increase in right lung areas and LHR. Severe forms of CDH showed less growth in right lung areas and LHR compared to milder forms of CHD and neonatal death was associated with no growth in right lung measurements.
June, 2015
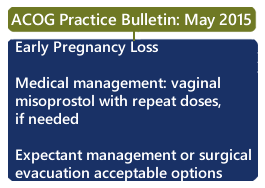
Early Pregnancy Loss. American College of Obstetricians and Gynecologists. Practice Bulletin No. 150. May 2015.
A new practice bulletin “Early Pregnancy Loss” has been published by The American College of Obstetricians and Gynecologists (ACOG). If medical management is indicated, 800 micrograms of vaginal misoprostol is recommended with a repeat dose, if needed. Expectant management or surgical evacuation are also acceptable treatment options. If the patient is Rh(D) negative and not sensitized, she should receive 50 micrograms of Rh(D) immune globulin immediately after surgical management or within 72 hours of a diagnosis of early pregnancy loss when expectant or medical management is planned.
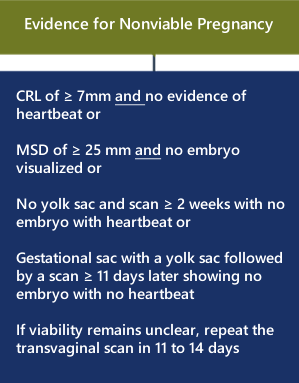
Early pregnancy loss diagnostic criteria are provided by transvaginal ultrasound during the first trimester.
Viability
Errors exist during the early first trimester in correctly assigning whether the pregnancy is viable, nonviable, or in an ectopic location. The false positive rate (incorrect diagnosis of a not viable pregnancy when the pregnancy is normal) is as high as 4.4%.
In a recent review, transvaginal ultrasound diagnosis of pregnancy failure in a pregnancy with uncertain viability is as follows:
CRL (crown rump length) of ? 7 mm and no evidence of heartbeat.
MSD (mean sac diameter) of ? 25 mm and no embryo visualized.
Initial scan shows a gestational sac without a yolk sac followed by a scan ? 2 weeks later demonstrating the absence of embryo with heartbeat.
Initial scan shows a gestational sac with a yolk sac followed by a scan ? 11 days later showing the absence of embryo with heartbeat.
If viability remains unclear, repeat the TVS in 11 to 14 days.
December 5, 2014
International standards for early fetal size and pregnancy dating based on ultrasound measurement of crown-rump length in the first trimester of pregnancy. Papageorghiou AT, et. al. Ultrasound Obstet Gynecol. 2014 Dec;44(6):641-8.
International standards are published for fetal size and pregnancy dating by crown-rump length (CRL) during the first trimester of pregnancy. This study included 4321 women with live singleton births from uncomplicated pregnancies. Eligibility criteria was from eight diverse countries with pregnancies recruited between 9 + 0 and 13 + 6 weeks. The study was designed to reduce methodical errors and to serve as an international standard for relating CRL to gestational age (GA). This entire article is open access for viewing and may be downloaded to obtain charts and tables related to CRL and GA. These charts are reproduced in the Normal First Trimester Exam under: International Standards for CRL and GA.
June, 2014
Ultrasound fetal imaging workshop. Reddy UM, et. al. Obstet Gynecol. 2014 May;123(5):1070-82.
A current commentary and executive summary on fetal imaging is presented as a result of a workshop hosted by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The workshop, representative of multiple organizations concerned with maternal and fetal health, reviews frequency and performance of MRI and ultrasound. Issues related to optimization of yield, costs, and research are reviewed. Useful recommendations are provided regarding soft markers observed during second trimester ultrasounds.
June, 2014
Diagnosis and treatment of fetal cardiac disease: a scientific statement from the American Heart Association. Donofrio MT, et. al. Circulation. 2014 May 27;129(21):2183-242.
The diagnosis and management of fetal cardiovascular disease is presented as a scientific statement from the American Heart Association and covers diagnosis of congenital heart disease, arrhythmias, and available treatment options. Cardiac anatomy, function, and rhythm are reviewed as well as the essentials of the fetal echocardiogram.
March, 2015
Imaging Characteristics for 13 Congenital Heart Defects
The following E-poster won Second Place in the “Obstetric Ultrasound: Fetal Anomalies” category at the 2015 Annual American Institute for Ultrasound in Medicine (AIUM) meeting, March 2015:
Cardiac Views and Imaging Characteristics
September 27, 2014
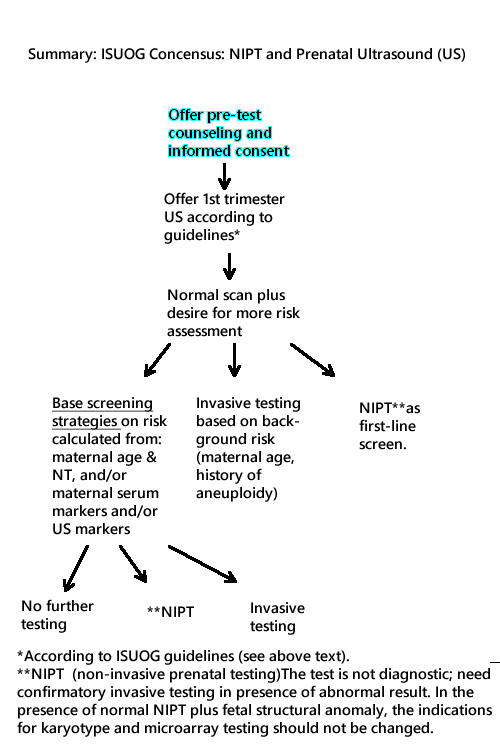
Non-Invasive Prenatal Testing (NIPT) and Prenatal Ultrasound Practice
The International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) recently published (June 3, 2014) a consensus statement on the topic of non-invasive prenatal testing (NIPT) as this new testing method relates to prenatal ultrasound practice. For details of this statement, please refer to the original document. [2]
In summary, women should be offered a 1st trimester ultrasound (US) (11 to 13 6/7 weeks) according to ISUOG recommendations [3] preceded by pre-test counseling.
The following is an algorithm summarizing a part of the ISUOG consensus statement.